
The technological advances in genetics and genomics now allows the full sequencing of exons and even the entire human genome (see ‘Related ObG Topics’ below). While WES and WGS have led to great advances in research and clinical genetics, use in pregnancy has remained controversial. While there is ongoing research on the topic of sequencing during pregnancy, the ISPD, SMFM and PQF have released a joint statement to provide guidance in the clinical prenatal setting.
The routine use of prenatal sequencing is not recommended, including cases where fetal DNA has already been obtained via amniocentesis, CVS or cordocentesis
The following are appropriate circumstances to consider prenatal sequencing in a non-research setting on a case-by-case basis
Consider the following minimal elements when providing education, counseling and informed consent
If providing pre-test counseling and informed consent, include the following in the discussion

In a normal heart, the pulmonary artery carries deoxygenated blood to the lungs. Oxygenated blood returns to the left side of the heart and the aorta then pumps the oxygenated blood to the rest of the body. In Transposition of the Great Arteries (TGA), the pulmonary artery and aorta have changed places (i.e., they are transposed). Therefore:
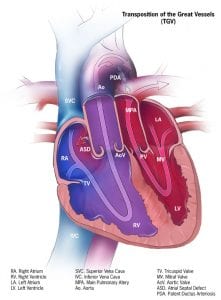
Image credit: Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities
CDC: Facts about dextro-Transposition of the Great Arteries (d-TGA)
Circulation-AHA journal: Transposition of the Great Arteries
CDC: Facts about Critical Congenital Heart Defects
Current diagnosis and treatments for critical congenital heart defects
Fetal Growth and Neurodevelopmental Outcome in Congenital Heart Disease
Please log in to ObGFirst to access this page